Abstract
Background: In the 52-week SUSTAIN study, which compared the P-selectin inhibitor crizanlizumab with placebo in patients with sickle cell disease (SCD), crizanlizumab 5.0 mg/kg significantly reduced the frequency of vaso-occlusive crises (VOCs) leading to healthcare utilization versus placebo (Ataga KI et al. N Engl J Med 2017;376:429-39). The overall incidences of adverse events and serious adverse events were similar among the patients treated with crizanlizumab and placebo.
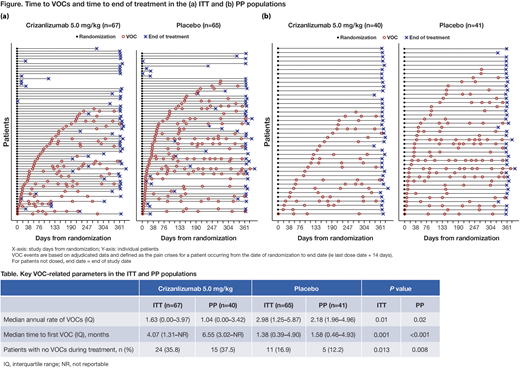
Aims: This post-hoc analysis from SUSTAIN evaluated key VOC-related endpoints in crizanlizumab 5.0 mg/kg and placebo groups in the per protocol (PP) population, as a way to assess the effect in patients who are able to follow the standard treatment regimen; data from the intention-to-treat (ITT) population will also be shown for context.
Methods: The SUSTAIN study was a randomized, double-blind, placebo-controlled, Phase II study (NCT01895361) that enrolled patients aged 16-65 years with SCD who had experienced 2-10 VOC events in the previous 12 months. Patients were randomized 1:1:1 to receive crizanlizumab 5.0 mg/kg, 2.5 mg/kg or placebo 14 times intravenously over 52 weeks; here we focus on the 5.0 mg/kg dose of crizanlizumab versus placebo. The number and time of VOCs leading to healthcare utilization (e.g., hospital admission, emergency department visit) from randomization to end of treatment were measured for each individual patient. Analyses were conducted on the ITT population (i.e., all patients randomized) and PP population (i.e., all patients randomized who received at least 12/14 planned doses of treatment, and completed the study without major protocol violations that impacted the efficacy assessments).
Results: In the crizanlizumab 5.0 mg/kg and placebo groups, there were 67 and 65 patients in the ITT population, and 40 and 41 patients in the PP population, respectively; the main reasons for exclusion from the PP population were associated with violations of the visit schedule. As shown previously (Ataga KI et al. N Engl J Med 2017;376:429-39), the median annual rate of VOCs was 1.63 in the crizanlizumab 5.0 mg/kg group versus 2.98 in the placebo group (stratified Wilcoxon Rank-Sum test, P=0.01; Table) in the ITT population. The median time to first on-treatment VOC was 4.07 versus 1.38 months (stratified log-rank test, P=0.001), respectively, in the crizanlizumab 5.0 mg/kg and placebo groups. Overall, 24/67 (35.8%) and 11/65 (16.9%) patients in the crizanlizumab 5.0 mg/kg and placebo groups (stratified Cochran-Mantel-Haenszel test, P=0.013), respectively, did not experience any VOCs during treatment. In the PP population, the median annual rate of VOCs was 1.04 with crizanlizumab 5.0 mg/kg versus 2.18 with placebo (P=0.02; Table). The median time to first on-treatment VOC was 6.55 months with crizanlizumab 5.0 mg/kg and 1.58 months in the placebo group (P<0.001). Overall, 15/40 (37.5%) and 5/41 (12.2%) patients in the crizanlizumab 5.0 mg/kg and placebo groups, respectively, did not experience any VOCs during treatment (P=0.008). The effect of treatment with crizanlizumab 5.0 mg/kg over placebo, as assessed by the three selected endpoints, is visible on the Figure, i.e., reduced frequency of VOCs, delayed first VOC, and increased number of patients with no VOCs during treatment.
Conclusions: This post-hoc analysis of SUSTAIN shows that crizanlizumab 5.0 mg/kg provided benefit over placebo: nearly halving the median annual rate of VOCs, doubling the time to first VOC, and doubling the number of patients with no VOCs during treatment in the ITT population. The effect was even more pronounced in the PP population. This suggests that the superior VOC-related treatment outcomes of crizanlizumab 5.0 mg/kg versus placebo are further improved in patients who are able to follow the standard crizanlizumab treatment regimen.
Kanter:NHLBI: Membership on an entity's Board of Directors or advisory committees, Research Funding; Apopharma: Research Funding; Pfizer: Research Funding; bluebird bio: Membership on an entity's Board of Directors or advisory committees, Research Funding; Global Blood Therapeutics: Research Funding; ASH: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; Sancilio: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding. Kutlar:Novartis: Consultancy, Honoraria, Other: Personal fees, Research Funding; Sancilio: Other: DSMB Chair; Bluebird Bio: Other: DSMB Member. Bruederle:Novartis: Employment. Shi:Novartis: Employment, Other: Stock owner of Novartis. Campigotto:Novartis: Employment. Ataga:Pfizer: Research Funding; Global Blood Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis Pharmaceuticals: Honoraria; Modus Therapeutics: Honoraria; Bioverativ: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.